How Much Does a Pulmonary Function Test Cost?
Last Updated on October 21, 2024
Written by CPA Alec Pow | Content Reviewed by ![]() CFA Alexander Popinker
CFA Alexander Popinker
A pulmonary function test, also called PFT or lung function test, is an essential non-invasive diagnostic exam that measures how efficiently the lungs are functioning through breathing exercises and measurements. But what price range can patients expect to pay out-of-pocket based on their insurance coverage, facility choices, specific tests ordered, and other cost factors?
While certainly not inexpensive, pulmonary function tests provide crucial quantitative data to accurately diagnose the presence and severity of certain respiratory conditions like asthma, COPD, pulmonary fibrosis, and more.
How Much Does a Pulmonary Function Test Cost?
On average, Pulmonary Function Test, PFT, costs range widely from about $40 on the low end for a simple spirometry screening to $600 or more for a comprehensive multilayered lung assessment.
On average nationally, PFTs tend to cost within these ranges depending on facility and region:
- Basic spirometry testing alone: $40 to $200
- Lung volume measurement tests: $100 to $350
- Lung diffusion testing: $150 to $500
- Maximal voluntary ventilation: $100 to $300
- Complete multilayered PFT assessment: $200 to $600+
Expect to pay on the higher end at large hospital labs versus independent outpatient centers which offer significant savings.
According to MDsave, prices for a PFT range from approximately $320 to $924. This pricing allows those with high deductible health plans or without insurance to purchase their procedures upfront, potentially saving money compared to traditional billing methods.
Another source, Health Street, lists their Pulmonary Function Test + Spirometry starting at around $180. The final price may vary depending on the selected package and any additional services requested during the checkout process, making it a flexible option for patients.
A report from AACMT indicates that their full pulmonary function testing is available for less than $300. They emphasize that costs can vary based on insurance coverage, but they provide estimates for out-of-pocket expenses prior to testing.
Why Are Pulmonary Function Tests Important?
Pulmonary function tests consist of breathing exercises and noninvasive procedures that assess how efficiently the lungs:
- Inhale and exhale air volumes.
- Transfer oxygen into the bloodstream.
- Utilize respiratory muscles.
Test results help:
- Accurately diagnose lung diseases and their severity.
- Monitor changes in chronic respiratory conditions.
- Evaluate lung health pre-surgery and occupational risks.
- Guide appropriate treatment plans tailored to each patient.
PFTs play a crucial role in managing lung health when performed properly.
Most Common Pulmonary Function Tests
You might also like our articles about the cost of a tuberculosis test, pectus excavatum surgery, or chest x-ray.
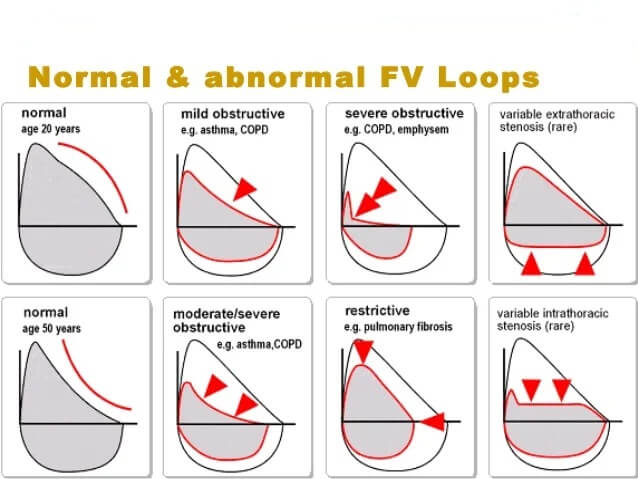
Spirometry – The most common PFT, measuring how much air a patient can inhale and exhale, along with flow rates. Helps identify obstructive disorders.
Lung Volume Tests – Measure total lung capacity, residual volume, etc. Indicates restrictive diseases.
Diffusing Capacity – Evaluates how efficiently oxygen is transferred from lungs to bloodstream. Flags diffusion issues.
Maximal Voluntary Ventilation – Assesses the maximum volume of air a patient can inhale and exhale per minute in a coached breathing exercise. Shows airflow limitations.
Doctors determine the right combination of pulmonary function tests required to thoroughly evaluate each patient’s respiratory status, needs, and diagnosis goals. This customization impacts costs.
Factors Influencing the Cost
- Testing Facility – Hospital-based lab versus lower-cost independent outpatient center or private pulmonology office. Hospitals tend to charge substantially more.
- Insurance Coverage – Insured patients save significantly over uninsured cash-pay individuals across the board through negotiated discounts. Out-of-pocket costs are lowered by plans but vary.
- Types of Tests Ordered – More advanced assessments like lung diffusion studies, volumes, and maximal ventilation cost more than basic spirometry screening alone. Complexity adds expenses.
- Provider Specialization – Some facilities charge a higher professional interpretation fee when results are evaluated by pulmonary specialists versus general technicians. Expertise costs extra.
- Geographic Region – Healthcare overhead like real estate, staffing, and equipment costs vary regionally. Urban areas with higher costs of living usually have higher PFT pricing.
Accounting for these key variables allows smart consumers to comparison shop and control costs through informed provider and testing decisions.
Hospitals vs. Outpatient Centers
Hospitals and academic medical labs tend to charge:
- Basic spirometry testing: $150 to $250
- Complete PFT assessment: $400 to $800
Independent outpatient centers and clinics tend to charge:
- Basic spirometry testing: $65 to $150
- Complete PFT assessment: $250 to $500
When feasible, having PFTs performed at outpatient centers saves 20% to 50% off hospital rates, considerably reducing out-of-pocket costs for patients.
Insurance Coverage
- Commercial Health Plans – Copays typically $20 to $75. Deductibles may also apply.
- Medicare Part B – Covers 80% of approved Medicare allowable amounts for medically necessary PFTs. Patients pay 20% copay plus Part B deductible.
- Medicaid & Medi-Cal – Little to no copay, fully covered. $0 to $10 out-of-pocket depending on state Medicaid program.
While costs vary by plan, having insurance through employers, Medicare, or Medicaid significantly reduces the burden of PFT expenses on consumers through negotiated discounts. Uninsured pay the most by far.
Make PFTs More Affordable
- Compare prices between local hospital labs versus independent outpatient diagnostic centers. Call and request quotes.
- Check if any nearby university medical facilities offer PFTs at reduced teaching rates. Worth investigating.
- Ask if community health clinics or county health programs offer PFTs on an income-based sliding scale.
- Inquire if payment plans, financial assistance, or flexible nonprofit programs are offered by facilities or lung associations if facing hardship.
- Consider at-home mobile spirometry options from telehealth companies that may be cheaper for basic lung assessments.
- Always verify in-network status of facilities within your plan’s provider network to minimize surprises.
Being a proactive and cost-conscious medical consumer goes a long way towards controlling PFT costs through informed choices. Seek help paying if needed.
When Are Pulmonary Function Tests Necessary?
PFTs play an indispensable role in effectively:
- Accurately diagnosing various lung diseases in their early stages before symptoms significantly worsen through objective testing. Everything from asthma to pulmonary fibrosis gets revealed through measured abnormalities.
- Determining surgical risk and guiding anesthesia approaches before procedures based on quantitative lung capacity data rather than just assumptions. PFTs provide exact cardiovascular reserve metrics.
- Establishing baselines and monitoring lung health changes over time for workers exposed to hazardous airborne particulates like coal or asbestos dust in occupational settings. Periodic PFTs flag lung function deterioration earlier.
- Adjusting medication regimens and treatment plans for chronic lung diseases based on measurable PFT changes at follow-ups indicating improving or declining health. Doctors rely on PFTs to make informed care decisions.
Across numerous vital purposes, pulmonary function tests provide vital objective data guiding optimal lung health management for both prevention and disease treatment. When indicated, PFTs are a wise investment.
Final Words
With out-of-pocket pulmonary function testing costs ranging widely from $40 to $800 or more depending on the facility, insurance coverage, tests ordered, and options chosen, patients and doctors can make prudent choices balancing affordability and clinical value.
Seeking in-network outpatient centers providing tests matched to medical need saves significantly while still delivering diagnostically accurate PFT results. Although expensive for some, pulmonary function tests enable life-improving prevention and treatment when lung health matters. Invest wisely in yourself.
Answers to Common Questions
How often should a pulmonary function test be done?
For conditions like COPD and asthma, doctors typically recommend repeat PFTs every 6 to 12 months to quantitatively track lung function over time and adjust medications and treatments accordingly. Frequency varies case-by-case.
Do you need to fast for a pulmonary function test?
No fasting or special diet is required leading up to basic PFTs. Patients should avoid strenuous exercise before exams. Inhaled bronchodilators may be withheld pre-test depending on the information needed. Ask your doctor about any medication or preparation concerns.
What will interfere with a pulmonary function test?
Recent exercise, smoking, or vaping before exams can affect results. Coughing or improper breathing technique when performing the tests also lowers quality. Patients should follow proctor instructions closely and give best efforts when inhaling and exhaling during procedures. Proper testing is essential.

Leave a Reply
Want to join the discussion?Feel free to contribute!